Are You Sleeping Enough? Diabetes And The Sleep Connection

As scientists better understand the elements that influence our health, they’ve discovered that numerous diseases are frequently seen together and can even aggravate one another. Poor sleep, for example, has been linked to diabetes, which can have severe consequences on your health.
Having one ailment often means you’re more likely to have the other. And each ailment can exacerbate the other in a variety of ways. If you experience type 2 diabetes or sleep problems, your doctor must look into the risk factors for the other condition so you can safeguard your long-term health.
Can diabetes cause a severe lack of sleep?
Sleep loss and insulin sensitivity have been associated in studies . People who don’t get enough out of their sleep cycle are wearier during the day and are more likely to eat comfort foods.
High blood sugar levels make it difficult to sleep.
Blood sugar levels that are too high can interfere with sleep. The high levels may be making it difficult for you to sleep — you may feel too hot, angry, or disturbed.
Another consideration is whether you need to go to the bathroom in the middle of the night. It can significantly impact your ability to obtain a good night’s sleep cycle if you regularly have high blood sugar levels. If this is the case, make sure to inform your medical professionals.
Tiredness during the day and after meals
If your blood sugar levels are high, you may feel tired all day, especially in the morning and after meals.
Tiredness will cause you to eat more, hoping to make up for the lack of energy. However, it will increase your blood sugar level causing a severe lack of sleep. Make a mental note of the figures and how you felt to understand the importance of good sleep .
Tiredness or lethargy could be a sign of low blood sugar if you’re on insulin or at risk of hypoglycemia, so it is imperative to check your blood sugar for that reason as well.
Hypoglycemia (low blood sugar) occurs while sleeping.
Hypoglycemia, or low blood glucose levels, might derange your sleep. You may be in danger of low blood sugar levels during the night if you take insulin or other blood sugar medications.
Low blood sugar levels at night can disrupt your sleep schedule, making it difficult to get out of bed in the morning and leaving you tired all day.
Hypoglycemia during the nighttime can be apparent, such as waking up overheated can sneak up on you. When evening hypoglycemia is detected, the treatment for it is usually straightforward.
If you’re having trouble matching the characteristics of a good night’s sleep or see signs of diabetic peripheral neuropathy, go to your doctor.
Diabetes and obstructive sleep
apnea (OSA)
People with obstructive sleep apnea have trouble breathing while sleeping. It is most frequent in adults aged 35 to 54 , significantly overweight, which might affect their capacity to sleep correctly at night.
Does sleep apnea affect diabetes?
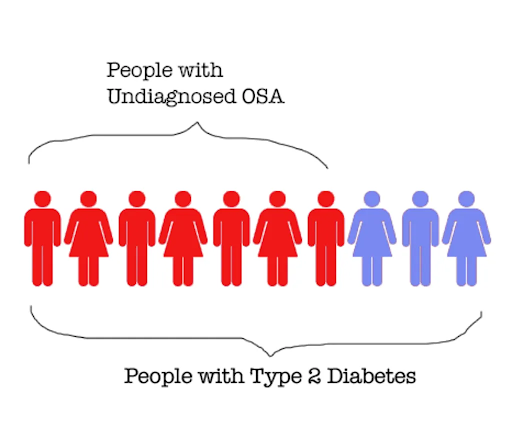
Sleep apnea and type 2 diabetes have a lot of connections. Some of them indicate how one ailment affects or exacerbates the other. Others point to shared risk factors or problems that can aggravate diabetes and sleep apnea.
For starters, both disorders have a risk factor: obesity. Obesity is one of the leading risk factors for type 2 diabetes because it alters how the body absorbs sugar. Obesity also appears to be a significant risk factor for developing obstructive sleep apnea (OSA).
Obesity is thought to be one of the leading causes of sleep apnea. It is because fatty tissue around the airways can make breathing difficult and uncomfortable.
Sleep apnea is also connected to the development of diabetes. When people’s sleep gets disrupted, their bodies’ capacity to metabolize sugar gets hampered. In studies , chronic exhaustion caused by poor sleep and diabetes is associated with blood glucose rises.

When thinking about sleep and its impact on diabetes, it’s vital to examine the amount of sleep and the quality, habits, and sleep patterns.
Despite mounting evidence tying sleep to diabetes, sleep issues are still an underappreciated aspect of the disease’s risk and treatment. Insulin and blood glucose levels are affected by a lack of sleep.
According to new research, insulin appears to have a daily cycle, like many other hormones and physiological systems. The body’s circadian clock, according to scientists, controls this cycle by regulating the time of insulin synthesis and secretion from the pancreas.
Circadian clock disturbances, which typically accompany sleep issues, appear to diminish insulin efficiency and, over time, lead to insulin resistance. Variations in insulin produce changes in blood sugar because insulin’s purpose is to control blood glucose.
Circadian rhythms related to sleep and diabetes can be disrupted by:
- Sleep patterns that aren’t consistent (like shift work, being a new parent, etc.).
- Sleep patterns are low in quality and disturbed (from the effects of your environment or use of caffeine).
- If you have sleep problems (insomnia and sleep apnea).
- Too much or too little sleep is a problem.
- Some tips to sleep well that can help your sleep hygiene include:
- Consistency is key. Every night and every morning, including weekends, go to bed and wake up at the same hour.
- Ascertain that your bedroom is calm, dark, soothing, and to a pleasant degree.
- Remove all electrical gadgets from the bedroom, including televisions, computers, and smartphones. Avoid huge meals, caffeine, and liquor before night.
- Make an effort to exercise. Physical activity during the day can make it easier to fall asleep at night.
Conclusion
It’s a good idea to discuss your risks with your doctor if you’ve been diagnosed with type 2 diabetes for tips to sleep well . Basic checks are available to determine whether you have one or both of these illnesses. You may build a plan to improve your sleep, metabolism, and overall health by gathering the necessary facts.
Authors:
Mrs.Sripriya Ravi, M.Sc, Senior Dietitian
Miss. Priyadharshini M.Sc, Dietitian